G.Nagarjuna Roll 49 internship assessment
Internship assessment
SCORING:
Feb 09,2023
Psychiatry Posting
From 12-12-23 to 26-12-23
Learned about importance of history taking and how by history we can reach to a provisional diagnosis.
- Saw different patients and learned how to take basic history
Examples like :
1. Schizophrenia
2.OCD
3.ALCOHOL DEPENDENCE SYNDROME
4. TOBBACO DEPENDENCE SYNDROME
5. Depression
6. Psychosis
7. Panic attack
- learnt the medications given to the patients and their side effects
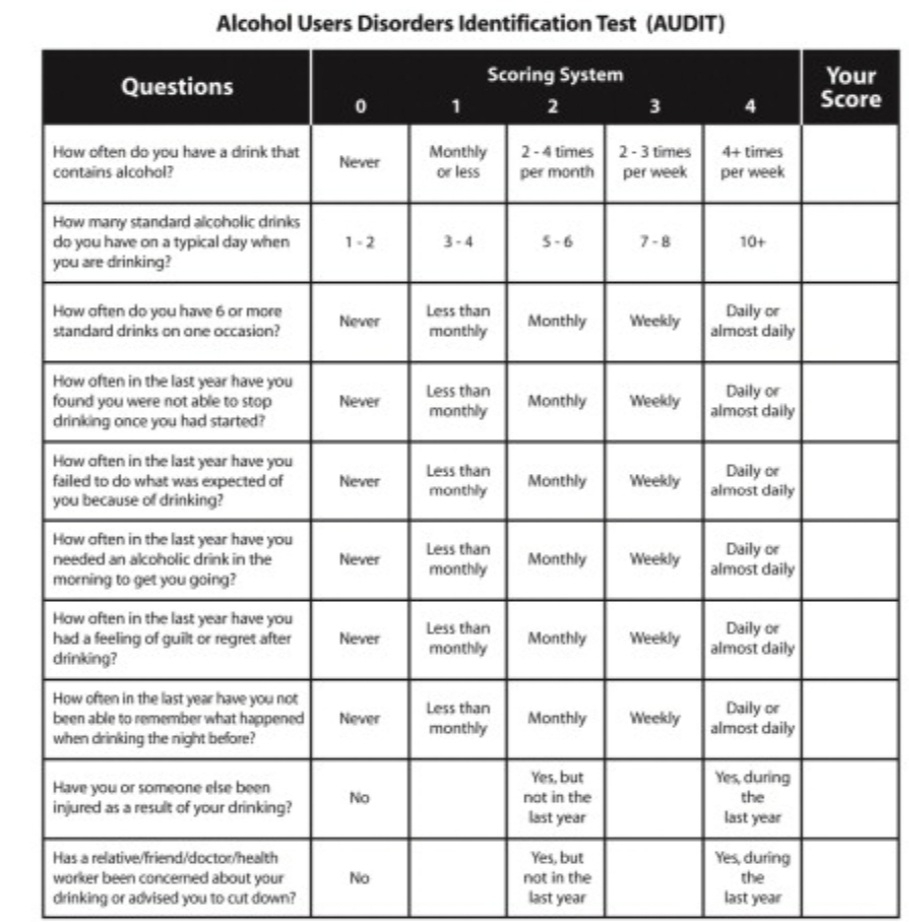
LEARNT ABOUT AUDIT SCORE WHICH IS PARAMETER IN EVALUATING ALCOHOL DEPENDENCE
SCORING:
0-7: SENSIBLE DRINKING
8-15:HAZARDOUS DRINKING
16-19:HARMFUL DRINKING
>20:ALCOHOL DEPENDENCE
Unit Duties
27-12-22 to 26-1-23
Case 1
A 50 year old male came to opd with
Chief complaints of abdominal pain
Q1) How Alcohol causes pancreatitis ?
Alcohol is believed to cause precipitation and increases the viscosity of pancreatic secretions, which leads to the development of protein plugs in the small ducts which then form calculi, causing progressive inflammation and fibrosis, which leads to loss of acinar, islet and ductal cells.
The pancreas uses oxidative and non-oxidative metabolism to process alcohol. The oxidative pathway leads to the formation of acetaldehyde, a reactive metabolite that causes detrimental effects in acinar cells through activation of stellate cells, increased expression of proinflammatory cytokines, and a decrease in NAD+/NADH ratios. The non-oxidative pathway requires the formation of fatty acid ethyl ester (FAEE) synthase, which leads to activation of key transcription factors, sustained increases in intracellular calcium, and inhibition of extracellular matrix proteins, ultimately leading to further cell injury .
Alcohol also leads to premature activation of trypsinogen and other digestive and lysosomal enzymes within the acinar cells themselves; this causes the pancreatic tissue to auto-digest and leads to further inflammation. Another contributing mechanism is intra-acinar activation of factor-kB (NF-kB), a transcriptional activator, which further drives the inflammatory response, which can cause up to 50% of pancreatic tissue damage and lead to severe, fatal inflammatory responses
Q2) What are the other causes Acute pancreatitis ?
Q3) what is the role NBM in treatment of acute pancreatitis patient's ?
A 26 year old female with C/O weakness in the lower limbs since 2 days
Q1) what is hypokalemic periodic paralysis ?
Hypokalemic periodic paralysis is a condition that causes episodes of extreme muscle weakness typically beginning in childhood or adolescence. Most often, these episodes involve a temporary inability to move muscles in the arms and legs. Attacks cause severe weakness or paralysis that usually lasts from hours to days.
Mutations in the CACNA1S or SCN4A gene can cause hypokalemic periodic paralysis. Mutations in the CACNA1S or SCN4A gene alter the usual structure and function of calcium or sodium channels. The altered channels are "leaky," allowing ions to flow slowly but continually into muscle cells, which reduces the ability of skeletal muscles to contract. Because muscle contraction is needed for movement, a disruption in normal ion transport leads to episodes of severe muscle weakness or paralysis.
Q2) How hypokalemia effects the heart function and what are Ecg changes can be seen in such patients?
Hypokalemia induces arrhythmia by two distinct mechanisms: direct inhibition of K+ conductance and indirect suppression of Na+/K+ ATPase activity. The latter results in intracellular Na+ accumulation. High intracellular Na+ reduces outward calcium (Ca+) current via Na/Ca exchanger, and as a result, increased intracellular Ca+ content and delayed after-depolarization occur. Cytosolic Ca+ activates Ca/calmodulin-dependent protein kinase II (CaMKII) by phosphorylation of the ryanodine receptor. Activated CaMKII stimulates late Na+ current (INa) and I-type Ca+ current (ICa-L) as well. This positive feedforward loop further increases the intracellular concentration of Ca+. High Ca+ is associated with pacemaker abnormalities. Subsequently, the final result is an altered repolarization process and prolonged AP duration, triggering early and delayed after-depolarization and risk of various types of arrhythmia.
Major causes of hypokalemia.
Excess renal loss
Mineralocorticoid excess
Primary hyperaldosteronism (Conn's syndrome) Glucocorticoid-remediable hyperaldosteronism
Renin excess
Renovascular hypertension
Bartter's syndrome Liddle's syndrome
Diuresis
Chronic metabolic alkalosis
Antibiotics
Carbenicillin
Gentamicin
Amphotericin B Renal tubular acidosis
Distal, gradient-limited
Proximal
Ureterosigmoidostomy
Gastrointestinal losses
Vomiting
Diarrhea, particularly secretory diarrheas
ECF →→ ICF shifts
Acute alkalosis
Hypokalemic periodic paralysis
Barium ingestion
Insulin therapy
Vitamin B₁, therapy
Thyrotoxicosis (rarely)
Inadequate intake
Case 3:
A 55 year old male patient came to the op with the cheif complaints of sob since 20 days.
Q)1. Which two conditions are associated with heart failure?
MI and chronic coronary artery disease. Both comprise the function of the ventricles. Or functionly a decrease in stroke volume and cardiac output Less common is heart failure due to lung disease.
Q)2. How is ventricle size related to heart failure?
The size and shape of the ventricle change with worsening heart failure. Inverse relationship exists between ventricular size and function.
Q)3. What is a normal heart ejection fraction? What does this mean? Ejection fraction (EF) refers to how well your left ventricle (or right ventricle) pumps blood with each heart beat. Most times, EF refers to the amount of blood being pumped out of the left ventricle each time it contracts. Normal: 55%-70%
Q)4. At which ejection fraction do we begin to see the effects of heart failure? 41-49% is borderline
Q)5. What are the causes of systolic and diastolic failure?
-Systolic Dysfunction (Ejection Fraction "EF" < 40%)
• AKA depressed EF
• Problem with the ventricle contracting • Decrease in stroke volume
Decrease in cardiac output
-Diastolic Dysfunction (EF>40%)
• AKA preserved EF
• Problem with the ventricle relaxing
• Caused by any process that decreases relaxation, decreases elastic recoil, or
increases stiffness of ventricle
Decrease in stroke volume
Q)6. List some common risk factors for heart failure.
• High blood pressure
• Coronary artery disease
• Heart attack • Diabetes
• Sleep apnea
• Congenital heart defects
• Valvular heart disease
• Viruses
• Tobacco use
• Alcohol use
• Obesity
Case 4:
Case5:
Procedure :
I have done Diagnostic tap for a patient having ascitis.
Sample was taken out and sent for analysis of the fluid.
And the SAAG value is found to be >1.1gm/dl. This suggest that the patient is having Portal hypertension cause is Chronic Liver disease
ABG:
ICU:
I checked vitals(BP,PR,RR,GRBS,SPO2, TEMPERATURE) hourly for patients in ICU.
I have seen some cases like
27 year old female whose diabetic and
And she is having hypertension.
When she is in icu her grbs is used to be
Between 300-400 and her BP used to be 180/100.
By continuous monitoring and informing our pgs about her situation. Giving Insulin
Continuous Infusion started at 6ml/hr then it is tappered slowly and she is final on inj glargine which is fixed dose.
A case of 50 year old female with left diaphragm paralysis. Her oxygen saturation was very low and she is continuously on ventilator. She is used to sleep on the side of diaphragmatic paralysis so that she can freely breath with other normal functioning right lung.
She is not cooperative to keep the mask
I Insisted her to place mask on the face
And explained the outcomes if doesn't wear the mask , she could land up in SOB.
Initially she is on 9 lit of o2 then her condition getting better it is tappered to 1lit of O2.
27 year old female whose diabetic and
And she is having hypertension.
When she is in icu her grbs is used to be
Between 300-400 and her BP used to be 180/100.
By continuous monitoring and informing our pgs about her situation. Giving Insulin
Continuous Infusion started at 6ml/hr then it is tappered slowly and she is final on inj glargine which is fixed dose.
A case of 50 year old female with left diaphragm paralysis. Her oxygen saturation was very low and she is continuously on ventilator. She is used to sleep on the side of diaphragmatic paralysis so that she can freely breath with other normal functioning right lung.
She is not cooperative to keep the mask
I Insisted her to place mask on the face
And explained the outcomes if doesn't wear the mask , she could land up in SOB.
Initially she is on 9 lit of o2 then her condition getting better it is tappered to 1lit of O2.
I took ABG samples 6 times for different patients and I learnt how to put Foley's catheter and Ryles tube insertion and did it on 4 patients
I took IV samples several times
Done CPR on 3 patients
WARD DUTY:
I made my co interns to put soap notes of various patients in the group
And did exam conducting duty
In exam duty I alloted different cases to students ,guided them to make blogs,filmed their presentation videos
As a ward intern I undertook the responsibility of a Bengal case and sent their samples,got various tests done,collected reports,collected their 2018 case sheet from MRD,talked to UROLOGY RESIDENTS,about the patient condition
NEPHRO DUTY:
I collected several patients samples,monitored vitals,collected reports.
I took the responsibility of patients, blood bank requisitions,talked to blood bank medical officer,helped patients to get their blood from blood banks and monitored the transfusion
I took patients for DIALYSIS and monitored them while they undergoing that process.