final examination short case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs".
This E log book also reflects my patient-centered online learning portfolio and your valuable comments on comment box is welcome.
MEDICINE CASE DISCUSSION:
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS :
50 year old male presented with weakness of lower limbs since 4days
VIEW OF THE CASE :
He had a history of fall 1 year ago and 4 months back when he developed pain in the right hip region, which was insidious in onset and intermittent at the beginning. Aggrevated on movement and relieved on rest and medication.
He went to the hospital 2 months ago when the pain progressed and became continuous, and was diagnosed with avascular necrosis of the femur due to a trauma to the hip one year ago and given medications.
4 days ago, patient developed weakness in the lower limb which progressed upto the hip.
He was taken to the hospital and was prescribed medications. On starting the medication, the weakness worsened.
The next morning, patient required assistance to walk and sit up but was able to feed himself. The weakness progressed so that by the evening he was unable to feed himself. He only responded if called to repeatedly.
The weakness was not associated with loss of consciousness, slurring of speech, drooping of mouth, seizures, tongue bite or frothing of mouth, difficulty in swallowing.
No complaints of any headache, vomitings, chest pain, palpitations and syncopal attacks.
No shortness of breath, orthopnea, paroxysmal nocturnal dyspnea, abdominal pain or burning micturition.
Past History:
No similar episodes in the past.
Patient is a known case of diabetes since 12 years. He is on insulin therapy
No history of hypertension, tuberculosis, epilepsy, asthma, thyroid and CAD.
No surgical history.
Personal History:
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and Bladder: Regular
No allergies
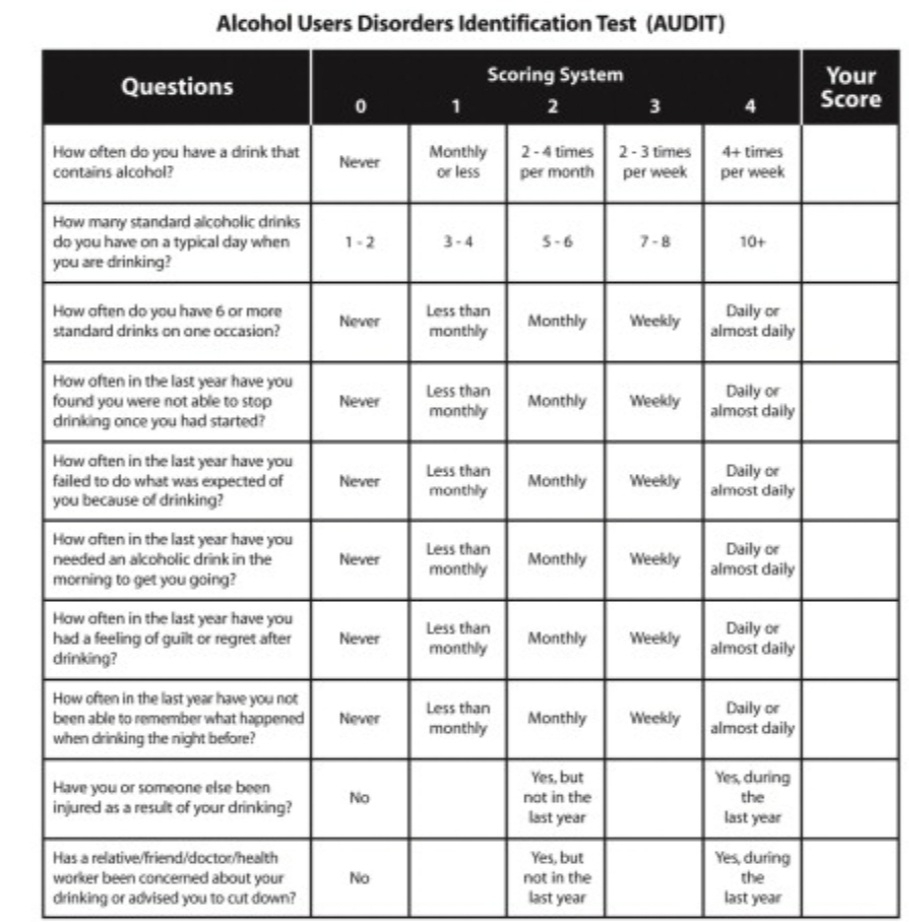
Addictions;
alcohol intake from 25 years 90ml per day
Started smoking from 10 years
Family History:
No similar history in family.
GENERAL EXAMINATION:
Patient is examined in a well lit room after taking informed consent.
Patient is conscious, coherent and cooperative.
He is moderately built and moderately nourished.
Pallor: Present
Icterus: absent
Cyanosis: absent
Clubbing: absent
No generalized Lymphadenopathy
Edema: present
Vitals:
Blood Pressure: 124/72 mmHg
Respiratory Rate: 17 cycles per minute
Pulse: 70 bpm
Temperature: Afebrile
Systemic examination:
▪CVS-- s1 ,s2 heard no murmurs
• Respiratory system- normal vesicular breath sounds heard
• Abdomen- no tenderness no palpable mass , not distended
On 03/06/2022:
c/c/c and afebrile
CVS - S1 S2+
CNS - Sensorium improved
P/A - soft and non tender
stools passed 4 days back.
On 04/06/2022:
c/c/c and afebrile
BP - 120/80mmhg
PR - 88bpm
CVS - S1 S2+
CNS - Sensorium improved
R/S - BAE + and LT CREPTS +
P/A - soft and non tender.
On 05/06/2022:
c/c/c
BP - 100/60mmhg
PR - 92bpm
CVS - S1 S2+
CNS - Sensorium improved
R/S - BAE + and LT CREPTS +
P/A - soft and non tender.
On 07/06/2022:
BP - 120/80mmhg
PR - 92bpm
Atrophy of right calf region
sensations of both limbs - intact
absence of mobility of both limbs
Provisional diagnosis:
Weakness Due to metabolic cause like hypokalemia
Investigations
On 03/06/2022:
ON USG
Rt kidney - 8.8 * 4.2 cm
Lt kidney - 10*3.6 cm
Size is normal but increased echotexture
CMD - partially maintained
Spleen - 12.9cm (increased)
FINDINGS ON USG
Multiple intraductal and parenchymal calcification noted in pancreas involving and head and pancreas.
8mm calculus noted in inferior pole of left kidney.
Distended gall bladder with calcification noted of 6mm.
IMPRESSIONS ON USG
• Cholelithiasis with GB sludge
• chronic pancretitis
• left renal calculus
• mild splenomegaly
• B/L grade - II RPD changes
• minimal ascitis
ECG :
on 02/06/22
on 02/06/22
electrolytes:
Potassium:2.5meq/L
Chloride:110meq/L
Sodium : 145 meq/L
Blood sugar: 195 mg/dl (on 02-06-22)
TREATMENT
on day 1
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) 2 amp KCL in 500ml NS slowly over 4-5 hrs
On day 2
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine
9) tab spironolactone
On day 3
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) proteolytic enema
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 4
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD
11) high protein diet
On day 5
1) tab ecospirin 70mg OD
2) tab atorvas 10mg OD
3) inj NS, RL at 70ml/hr
4) syrup potchlor 15ml/po/tid
5) normal oral diet
6) inj HAI - TID
7) tab ultracet 1/2 po/ QID
8) syrup cremaffine plus 15ml/po/od
9) tab spironolactone 25mg/po/od
10) tab azithromycin 500mg OD